#945: The Long Goodbye
It was my original intention that this week’s essay would be about Robert F. Kennedy, Jr., who as of about a month ago, is an announced candidate for the Democratic nomination for President. Towards that end, I read up on him, the place he occupies in his famous family, the books and articles he has published over the past 30 years, his work as both an environmental lawyer and “position” as one of the nation’s leading conspiratorial “anti-vaxxers,” and his stances on a wide range of political issues. My main interest in writing about him was trying to figure out how a person with his pedigree (not to mention troubled life) could even consider running as a political “outsider." I mean, the dude’s a Kennedy for crying out loud. Then too, I was (and still am) fascinated by how one moment Junior can come off as an ultra-right wing populist with a conspiratorial streak that would please the likes of a Roger Stone or Steve Bannon, and the next sound like a Kennedy - a progressive friend of the masses.
Actor Bruce Willis: Now in the throes of FTD
But after reading journalist Rebecca Traister’s masterful piece, RFK’s Inside Job in the June 30th issue of New York Magazine, I changed my mind; Ms. Traister had written - and far, far better than I could ever hope - the piece I had in mind. And so, wishing to clear my mind of RFK, I instead aimed my brain towards my twice-weekly Institutional Review Board (medical ethics) material. And there, right before my eyes, was an announcement from the FDA that it has just granted full approval to Leqembi (l’-kem-bee), the first drug to clearly, but modestly, slow the progress of Alzheimer’s Disease (A.D.). And suddenly, it came to me: I would write about this medical mini-breakthrough . . . the very kind of thing that RFK, Jr. might well understand to be part of a conspiracy to endanger dementia sufferers while enriching “big pharma.”
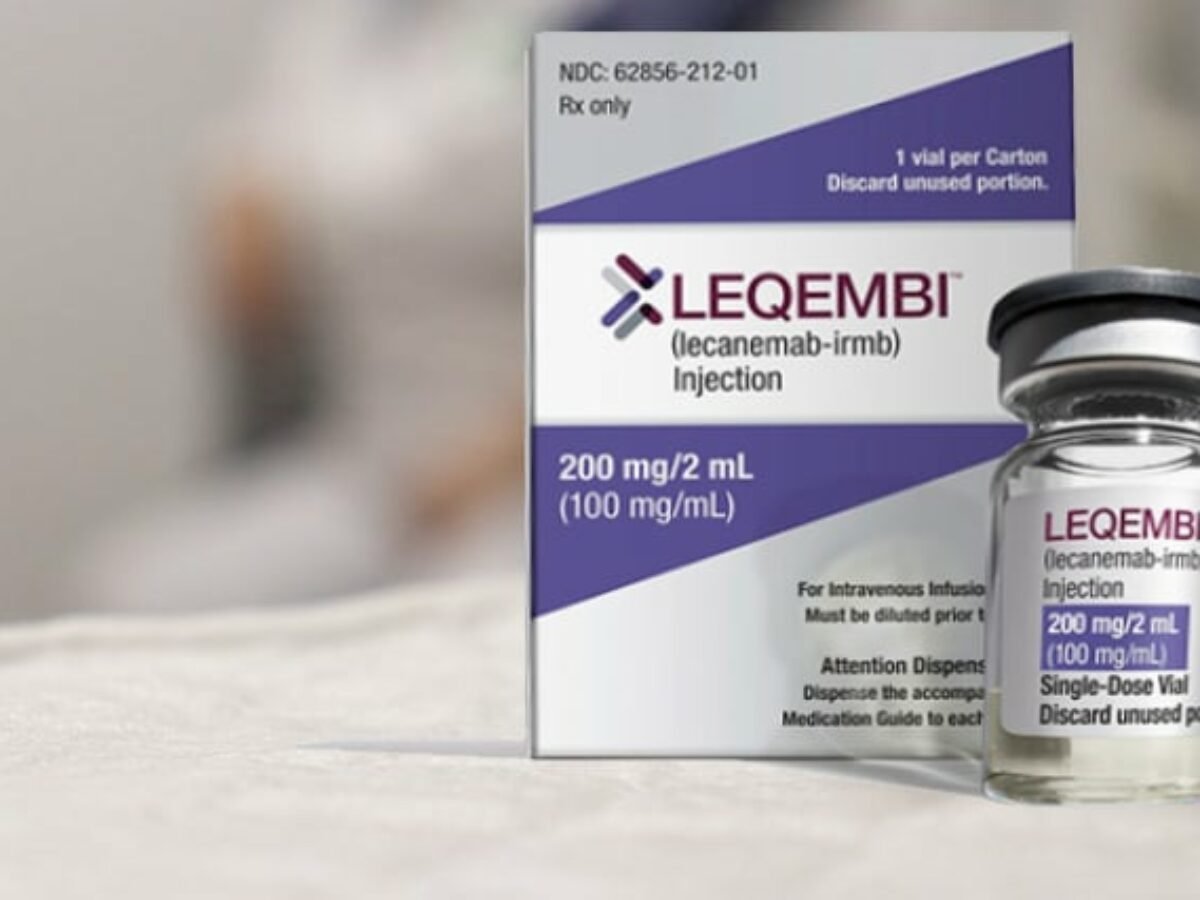
Leqembi (LECANEMAB-IRMB), co-researched and manufactured by the pharmaceutical company Eisai in Tokyo and Biogen in Cambridge, Mass., is a monoclonal antibody (a lab-made protein), that targets amyloid beta in the brain. (Don’t worry if you don’t know what amyloid beta means; there isn’t going to be a test at the end of this essay. All you need to know is that A.D. is largely caused by the build-up of “plaque” in brain, and that plaque is largely made up of amyloid beta. And by the way, all those drugs whose names end in mab . . . this stands for “monoclonal antibody”).
Dementia is an umbrella term used to describe a range of neurological conditions affecting the brain that get worse over time. As of today, none can be cured, let alone slowed. Of all the various forms of human dementia (estimated to be as many as 400), the very worst (and least-known) are:
Creutzfeldt-Jakob disease (CJD) which causes a type of dementia that causes personality changes, anxiety, depression, and memory loss, usually within a few months.
Dementia with Lewy Bodies: a type of progressive brain disorder in which Lewy bodies (abnormal deposits of a protein called alpha‑synuclein) build up in areas of the brain that regulate behavior, cognition, and movement.
Huntington’s Disease, (“Woody Guthrie Disease”): a progressive brain disorder caused by a defective gene. This disease causes changes in the central area of the brain, which affects movement, mood and thinking skills;
Frontotemporal Dementia (FTD): One day this will likely be known as “Bruce Willis Dementia.” FTD refers to a group of disorders caused by progressive nerve cell loss in the brain's frontal lobes (the areas behind the forehead) or its temporal lobes (the regions behind the ears). For many, the initial diagnosis is Aphasia, a disorder that results from damage to portions of the brain that are responsible for language. Before he was diagnosed with FTD, Mr. Willis announced his retirement due to an inability to remember - let alone pronounce - the words of a movie script.
The type of dementia which afflicts the greatest number of people world-wide is Alzheimer’s. According to the Alzheimer’s Association, more than 6 million people in the United States alone are living with the disease.
Each of these forms of dementia (and oh so many others), have their own foundations which support research. Many of these afflictions have clinical trials in progress. They are underwritten by these foundations, by wealthy family members of people suffering from these illnesses, by university med schools, by for-profit pharmaceutical companies, and the federal government. According to Clinicaltrials.gov, the U.S. National Library of Medicine, there are currently 3,158 ongoing studies into A.D. alone. These range from Phase I to post-marketing studies. All are seeking the same thing: to lessen, abate and eventually one day find a cure for this disease. The most sophisticated of these studies are randomized (subjects are chosen by a computerized “flip of the coin”), double-blind (neither the subject nor the medical investigators know which dose the participants are receiving), and placebo-controlled (in which a “dummy lookalike drug” is used in order to determine whether or not the drug being investigated is potent).
Returning to Leqembi, the newest FDA-approved drug for A.D. Studies show that it has slowed cognitive decline by 27 percent over 18 months compared with a placebo (a dummy, lookalike drug). This represents a five-month delay in progression — dismissed as negligible by some but hailed as a milestone by others for a malady that has, up until now, been largely untreatable. Not surprisingly in this day and age, there are naysayers who only talk about Leqembi’s potential side effects (“adverse events” in medicalese). Skeptics also note that the drug’s effectiveness is limited — perhaps too subtle to be noticed by a patient — and that the medication can cause potentially dangerous brain swelling and bleeding. The drug is expensive — $26,500 per year. And Medicare is imposing conditions on coverage, a move fueling a bitter battle between government officials and advocacy groups.
At present, it appears that Medicare enrollees in the Original Medicare will have to pay a co-payment of 20% of the cost of the drug, after meeting their deductible. This means that people on Original Medicare could pay about $5,000 out of pocket annually for Leqembi, according to health-care research group KFF. Medicare Advantage enrollees typically pay 20% of a drugs' costs, up to their plan's out-of-pocket maximum, KFF noted, which means that people on these plans may also face high out-of-pocket costs for the medication.
All drugs and procedures have potential side effects; by law they must be made known to subjects in clinical trials and when approved, to all those who will be taking the medication. For a segment of society, the fact that Leqembi (or any other medicine) has side effects is unacceptable. That’s where conspiracies come in. (It should be noted that the most-cited of these Leqembi adverse events was “brain bleeding” (ARIA — amyloid-related imaging abnormalities). Upon further investigation it turned out that many who had this problem (which is, generally has few - if any - visible symptoms) were taking blood-thinning medications such as Plavix (clopidogrel) and Coumadin (warfarin). Once the blood-thinning dosages were lowered or eliminated, the incidence of ARIA lessened.
Remember all those - including RFK, JR. - who claimed - against all credible medical proof - that the MMR (Measles, Mumps, Rubella) vaccine caused autism in children? Despite being thoroughly disproven and discredited by medical researchers around the globe, there are still people who firmly believe that the vaccine is all part of a conspiracy. The same is true with virtually every COVID-19 and SARS (Severe Acute Respiratory Syndrome) vaccine approved for use over the past several years. Let’s face it: no medicine, whether taken orally, injected just under the skin (sub-Q) or infused (IV) is 100% safe. Why? Because subjects and patients, like the people who do research, are human beings . . . less than perfect. And many times subjects and patients have other things wrong with them (these are referred to as “comorbidities”) which may or may not cause a pill, shot or infusion to create a problem. But even if a small percentage suffer a problem - such as diarrhea, hair-loss or even, God forbid, death, what about the nearly 95+% who find improvement? Are we to put huge roadblocks along the path to improvement - if not eventual recovery - because of the very, very few?
Alzheimer’s disease and other pre-senile dementias are often referred to as “the long goodbye.” It is an apt expression, which also happens to be the title of a 1953 Raymond Chandler novel starring his L.A. detective Phillip Marlowe. As anyone who has ever watched a loved one slip into the shadows of dementia, they know what it feels like to be left facing and caring for a stranger with a familiar face. It is a pain far worse than a spinal tap. In an era where people without a stick of real medical knowledge or a single unit of scientific study (save, perhaps a 3-unit class in Biology 1), there are many megaphoned maniacs getting a growing segment of the public to believe that clinical research is a “zero-sum game” between patients and profit. This is the last thing people suffering from HIV, dementia, cancer, or any of a host of horrifying diseases need.
What we need now, more than ever, is hope . . . not hysteria.
Perhaps I’ll write a future essay about RFK, Jr. after he’s gotten over his current manic obsession with becoming President of the United States. Until then, I will pray for his health and for the health of all the doctors, nurses, pharmacologists, biomechanics, and medical ethicists who are daily engaged in the art and science of healing.
Copyright©2023 Kurt Franklin Stone